This
article was originally published on Canadian Blood Services’ RED blog on
Thursday, May 17, 2018
Author: Dr. Geraldine Walsh
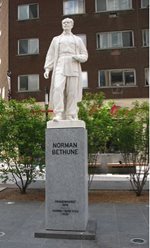
On April 10th, 2018, the
Centre for Blood Research presented its 8th Annual Norman Bethune Symposium. This event honours Canadian physician, Dr. Norman Bethune, who in the 1930s spearheaded the implementation of the earliest practical mobile blood collection and distribution systems.

During his introductory remarks,
Dr. Ed Conway, director of the Centre for Blood Research, and a Canadian Blood Services’ adjunct scientist, reminded the audience that this event takes advantage of some fascinating Canadian medical history. Dr. (Henry) Norman Bethune was born in Gravenhurst, Ontario in 1890. Bethune followed in the footsteps of his grandfather, a doctor who had been instrumental in founding the University of Toronto medical school. During the First World War, Bethune interrupted his studies to join the Canadian Army and serve as a stretcher-bearer in France. After recovering from shrapnel injuries sustained at the front, Bethune returned to Canada and completed his medical studies, graduating in 1916 (alongside Dr. Frederick Banting, another Canadian doctor destined for induction into the Canadian Medical Hall of Fame).
Creative and controversial, an innovator and a revolutionary, Bethune was an undoubtedly complex character. During the early years of his medical career in Canada and the US, Bethune invented or redesigned a dozen medical and surgical instruments, and innovated several surgical techniques. Practicing medicine during the Great Depression, Bethune became disillusioned with socio-economic inequality, and was an early and outspoken proponent of universal access to health care. He was also a communist who supported the loyalists during the Spanish Civil War and Mao Zedong’s Chinese Communists during the Second Sino-Japanese War. Working at the front lines of these conflicts, he helped establish an early mobile blood transfusion service, performed battlefield surgeries, and trained other doctors and nurses.
In November 1939, Dr. Bethune died of blood poisoning, contracted after cutting his finger during a battlefield surgery in China. Virtually unknown in Canada in his lifetime, Bethune was celebrated in China, where he was eulogized by Mao Zedong in a text that became compulsory reading. Bethune’s accomplishments and his influence on trauma surgery remain relevant today.
The program
The program for this year’s symposium, put together by Dr. Conway and
Dr. Dana Devine, a professor at the UBC Centre for Blood Research and Canadian Blood Services’ Chief Scientist, perfectly reflected and celebrated Bethune’s legacy of innovation.
On military applications
The day began with a talk by Lieutenant-Colonel Andrew Beckett MD. A trauma surgeon with the Royal Canadian Forces Medical Services and a researcher at McGill University, Dr. Beckett set the stage for the day, calling Bethune a controversial visionary, and described how his ghost continues to guide casualty care to this day.
Working as a surgeon at the frontlines of conflict, Bethune would have dealt with horrendous injuries. He recognized that the best hope of saving lives was to start treatment as early as possible, stating that “Doctors must go to the wounded – and the earlier, the better”. In the case of massive trauma, patients often die within 30 minutes of injury due to blood loss. As Bethune recognized, resuscitation with blood products must begin as soon after injury as possible, to reduce shock and give the best chance of survival.
Providing a moving and very personal patient perspective, the importance of intervention as soon as possible after massive injury was poignantly illustrated by Colleen Fitzpatrick, who spoke about the life and death of her son, Darren. Aged 21, Cpl. Darren Fitzpatrick died of injuries sustained while serving with the Canadian Forces in Afghanistan. Caught in an explosion, Darren received immediate treatment on the ground and was later flown to Germany. Seriously injured, Darren spent two weeks receiving treatment in Germany, with his family by his side, before being flown home to Canada where he died.
In telling her heartbreaking story, Colleen expressed how grateful she is that she got to spend those last few precious days with her son. Due to the transfusions and interventions that prolonged Darren’s life, she got to say goodbye, a chance many families of fallen soldiers do not have. She has become an advocate for blood donation, and her family has organized blood drives in Darren’s name.
To provide critical early intervention, blood products need to be available at the front lines, despite logistical and environmental challenges. This is one focus of Dr. Beckett’s research work. In collaboration with Canadian Blood Services, Dr. Beckett described work he has done to test blood products subjected to the harsh conditions they would experience when being transported in austere environments, to ensure that the products remain suitable for transfusion (for more on this, see:
Battlefield blood drops – getting blood farther forward as safely as possible). Canadian Blood Services and the Canadian Armed Forces also collaborate to ensure the military has the products they need, when they need them. For example, Canadian Blood Services has reinstated a whole blood program for the military based on recent evidence of improved outcomes in certain situations when whole blood is transfused rather than individual components.
Due to logistical and environmental constraints, militaries often have simplified versions of collection and transfusion protocols. As Dr. Beckett noted, some of these approaches, based on current knowledge and evidence, reflect exactly the approaches applied by Bethune over 80 years ago, further exemplifying his visionary approach and continued relevance.
“Drs. Devine and Conway are to be congratulated for bringing together engaging and interesting speakers, and Dr Beckett’s opening comments about Norman Bethune and his legacy marvelously set the stage by creating the context for thinking innovatively from bench to bedside. The powerful patient perspective poignantly brought home the compelling human reason for the work we do. I am very proud to have joined a team of current and future thought leaders in blood research whose work makes such a profound difference.”
Dr. Isra Levy, VP Medical Affairs and Innovation, Canadian Blood Services
There were many fantastic talks at the symposium, including opportunities for students to present their work. To read a description of all the presentations, visit the
Centre for Blood Research blog. A few were particularly relevant to Bethune’s legacy.
 On new and improved products
On new and improved products
Several excellent talks described new or improved blood products, that could have applicability to both civilian and military medicine. Dr. Jose Cancelas from the University of Cincinnati described his work to understand how best to cold-store platelets. Currently stored at room temperature for up to seven days, if platelets could be cold-stored and maintain their function once transfused, the availability of these life-saving products could be improved.
Dr. Steven Spitalnik from the Columbia University Medical Center described “Making better red blood cell donors”, a talk which asked some fascinating questions. Blood products are complex biologics that come from individual donors – can they be turned into pharmaceuticals? Can we understand and manage the individual differences inherent in blood products? Some red blood cell units store better than others – they maintain higher quality over the storage period before transfusion. Why is this? To begin to approach these questions, Dr. Spitalnik described work looking at various donor factors (e.g. genes, diet, environment) and their impact on red blood cells to determine how we might begin to understand what makes the ideal red blood cell unit.
On a related theme, Dr. James Zimring (Bloodworks Northwest) gave a characteristically humorous yet informative talk on platelets for transfusion. His work links platelet metabolic markers with data on how well platelets function after transfusion (24-hour recovery and survival of platelets after transfusion). One objective of this approach could be to determine which donors might produce the most effective platelets; however, Dr. Zimring acknowledged the limitations of the data and challenges that remain in its interpretation.
Canadian Blood Services and its Centre for Innovation are proud to partner with the Centre for Blood Research to deliver training and education events including the annual Norman Bethune Symposium.
On pushing boundaries
Continuing Bethune’s legacy of innovation, several talks demonstrated how the boundaries of transfusion medicine continue to be pushed and expanded. Dr. Peter Zandstra (University of British Columbia) talked about engineering blood stem cells. He described the challenges and successes of expanding and manipulating these cells in a laboratory setting, using automated bioreactors. As they continue to develop these technologies, the goal is to use laboratory-expanded cells to provide more effective stem cell treatments for more diseases.
Dr. Celina Montemayor Garcia (National Institutes of Health) gave a fascinating talk on the use of next generation sequencing to interrogate the intricacies of red blood cell antigens. Using this approach brings transfusion medicine into the realm of “big data”. Dr. Marco Marra (University of British Columbia) described another “big data” research project – BC Cancer’s Personalized Oncogenomics Project. A truly exciting approach, it represents the integration of patient, treatment, clinical and personalized genomic information to support real-time cancer treatment decisions. Dr. Marra presented some promising results from this project, which aims use genome knowledge to lead to better outcomes for patients.
On education and innovation
Bethune was an educator as well as an innovator, and Dr. Yulia Lin’s (University of Toronto) presentation reminded the audience of the importance of continuous transfusion education. Transfusion is somewhat unique in that it crosses many fields and disciplines – doctors who are not necessarily experts in transfusion must prescribe transfusion products in their practice. Dr. Lin described her involvement in several initiatives at undergraduate and postgraduate levels that train transfusion prescribers to use blood products as appropriately as possible (learn more
here.) Dr. Lin emphasized the importance of auditing and feedback to understand and ensure continuous education programs are having an impact.

 An inspiring day
An inspiring day
After the event, I had the opportunity to speak with Dr. Isra Levy, Canadian Blood Services Vice President, Medical Affairs and Innovation, about his impressions of the day. He told me it was his first time attending, and that he found it enjoyable in every sense. Dr. Levy described the 2018 Symposium as a collegial and stimulating day to network, to learn and to be inspired.
“I was struck by the level of engagement of the participants, the high quality of the presentations and speakers, the coherence of the program and its subtle but effective construct such that it was relevant and interesting to clinicians, scientists, clinician scientists and students alike. It is clearly a venue that helps trainees connect with each other and with mentors, and provides experience as well as information that will stand them in good stead for the rest of their careers.”
Dr. Isra Levy, VP Medical Affairs and Innovation, Canadian Blood Services
A perfect summation of a symposium that was inspiring and informative. Well done to all those who spoke and participated and congratulations to the organizers.
Photos courtesy of the Centre for Blood Research; Norman Bethune Statue image: Place Norman Bethune, Montreal, by Gary Soup is licensed under the Creative Commons Attribution 2.0 Generic license.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.